
PTA BALLOON COMPARISON STUDY
Crawford J, Gasparis A, Kim P, Jotwani M, Banerjee S, Labropoulos N.
Journal of Vascular Access. 2020.
Procedural Comparison of a Standard PTA Balloon for Fistula and Graft Maintenance Procedures with the Novel Chameleon™ PTA Balloon Catheter
SUMMARY
34.2%
Procedural Time Reduction1,†
27.7%
Fluoro Time Reduction1,†
49.1%
Contrast Volume Reduction1,†
The Chameleon™ PTA balloon catheter can reduce procedure time, fluoroscopy time, and contrast volume. This could help provide a more efficient procedure with simpler, more intuitive solutions that combine angioplasty and imaging in one device.
STUDY OVERVIEW
PATIENT STATISTICS
Sample Size (n) = 68
Group A = 34
(Standard PTA)
Group B = 34
(Chameleon™ PTA balloon)
- No significant gender differences between groups
- Comorbidities were similar to national rates in both groups (hypertension, coronary artery disease, and diabetes)
OUTCOMES
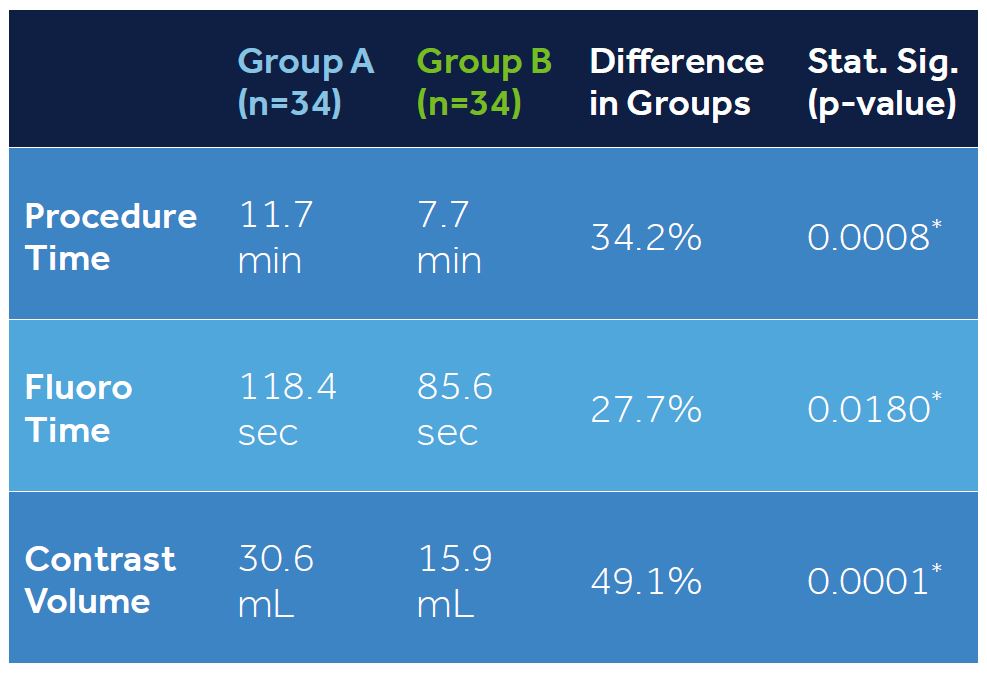
Comparison of outcomes between a standard PTA balloon (Group A) and a Chameleon™ PTA balloon (Group B) using multiple regression corrected for lesion location and length.
* Statistically significant per multiple regression.
1 Crawford J, Gasparis A, Kim P, Jotwani M, Banerjee S, Labropoulos N. Procedural comparison of a standard PTA balloon for fistula and graft maintenance procedures with the novel Chameleon™ PTA balloon catheter. J Vasc Access. (2020 Dec 15). doi: 10.1177/1129729820979479.
© 2020 Medtronic. All rights reserved. Medtronic, Medtronic logo and Further, Together are trademarks of Medtronic. All other brands are trademarks of a Medtronic company. 12/2020 – US-RC-2000075
Indications for Use
The Chameleon™ PTA Catheter is indicated for use in Percutaneous Transluminal Angioplasty of the femoral, iliac, and renal arteries and for the treatment of obstructive lesions of native or synthetic arteriovenous dialysis fistulae. The Chameleon enables the infusion of diagnostic or therapeutic fluids. This catheter is not for use in coronary arteries or cerebral vasculature.
Contraindications
DO NOT use the Chameleon™ Device: For coronary arteries nor for the delivery and/or expansion of stents. In patients who cannot tolerate anticoagulation therapy.
Warnings
Single patient use only. Do not re-use, re-process or re-sterilize.
Use the recommended balloon inflation medium. DO NOT use air or any other gaseous medium (e.g. CO2) to inflate the balloon or for infusion through the catheter.
When the catheter is exposed to the vascular system, it should be manipulated only while under high-quality fluoroscopic observation.
- DO NOT manipulate the catheter unless the balloon is fully deflated. Never advance / withdraw against any resistance. DO NOT use excessive force. If resistance is felt, determine the cause and take any necessary remedial action. Applying excessive force to the catheter may lead to tissue trauma and / or device damage.
- DO NOT exceed the RBP recommended on the product label. Balloon rupture may occur if the RBP rating is exceeded. To prevent over pressurization, use an inflation device with manometer.
Precautions
- Only physicians trained in the performance of PTA procedures should use the Chameleon™ device.
- The minimal acceptable sheath French size is printed on the product label. DO NOT attempt to pass the catheter through a sheath size smaller than that indicated on the product label.
- The recommended guide wire size is printed on the package label. DO NOT attempt to use the catheter without a guide wire or with a different size other than the one indicated on the label.
- If resistance is felt during post procedure withdrawal of the catheter, confirm that the balloon is fully deflated and only then remove the balloon catheter, the guide wire and the introducer sheath as a single unit.
Potential Adverse Reactions
Complications from a peripheral balloon dilatation procedure may include:
- Aneurysm or pseudo-aneurysm.
- Arrhythmias.
- Embolization.
- Hematoma.
- Hemorrhage, including bleeding at the puncture site.
- Hypotension / hypertension.
- Occlusion.
- Pneumothorax or Hemothorax.
- Sepsis / infection.
- Short term hemodynamic deterioration.
- Stroke.
- Thrombosis.
- Vessel dissection, perforation, rupture or spasm.
